Medi-Cal Eligibility Requirements
Medicaid Requirements in California
Navigating health care can be challenging, but understanding California Medicaid eligibility requirements is the first step to affordable coverage. Known as Medi-Cal, this program provides free or low-cost health care to millions of Californians, including families, seniors and those with disabilities. People who have certain conditions, such as tuberculosis and HIV, might also qualify for Medi-Cal — eligibility is based on factors like income, household size and specific needs.
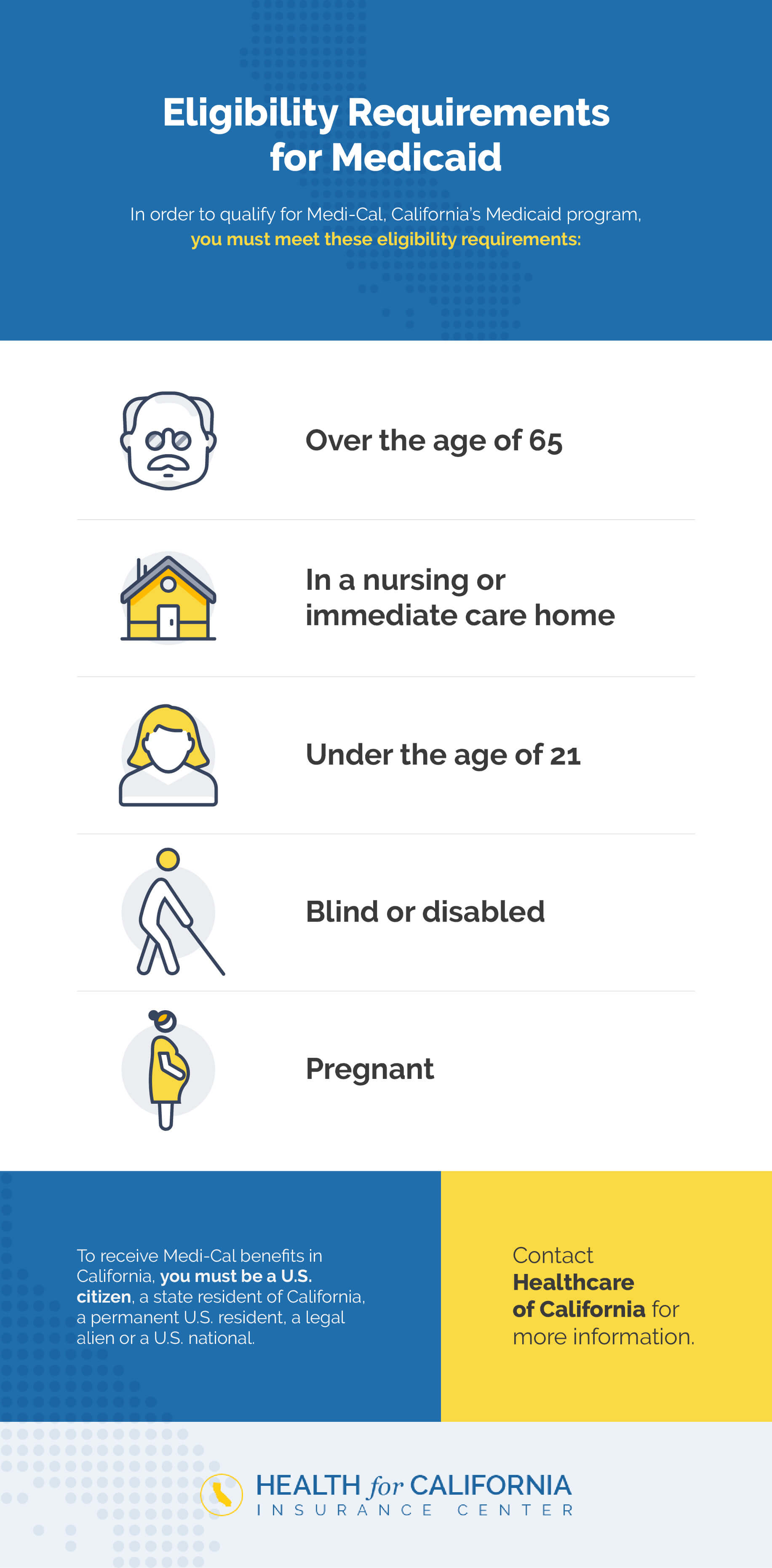
Who Is Eligible for Medicaid in California?
California residents who are United States citizens, permanent residents, legal aliens or U.S. nationals are eligible for Medi-Cal. There are several ways to qualify for the program. Some individuals qualify based on their household income level, while others meet specific requirements concerning their health status or age. You may be eligible if you are:
- Over the age of 65.
- Blind or disabled.
- Pregnant.
- In a nursing or intermediate care home or a skilled nursing facility.
- Under the age of 21.
- A refugee living in the U.S. temporarily.
- A recipient of either cervical or breast cancer screening.
Parents and Legal Guardians

As a parent or guardian relative of a child who is under the age of 21, you may be eligible for Medicaid assistance if you are caring for a child whose parents:
- Have passed away.
- Do not live with the child.
- Are incapacitated.
- Are unemployed.
An Addition to Existing Benefits Programs
If you qualify for Medi-Cal benefits, you may also qualify for additional assistance programs and vice versa. You will likely qualify for Medi-Cal benefits if you are enrolled in and receive benefits from any of these programs:
- CalFresh: CalFresh is California’s food stamp program, and the federal version is the Supplemental Nutrition Assistance Program (SNAP). Eligibility for CalFresh is based on income and monthly expenses.
- Supplemental Security Income (SSI) and State Supplementary Payment (SSP): The SSI program provides supplement income monthly to adults who meet certain requirements, such as being blind, over the age of 65 or disabled. SSP is California’s version of SSI.
- CalWorks (AFDC): This program provides cash assistance to families with children. Eligible families receive cash monthly to help them pay for food, housing and other needs. Eligibility is based on income, age, resources and citizenship status.
- Refugee Assistance: California’s Refugee Assistance program is designed for refugees who don’t have children and have no other form of assistance. The program provides employment assistance to help people gain self-sufficiency.
- Foster Care or Adoption Assistance Program: The California foster care and adoption assistance program is designed to help people adopt a child. The children who are eligible for the program would otherwise have remained in long-term foster care.
What Are the Medi-Cal Eligibility Requirements for Families?
Usually, if you’re eligible for the programs above, you meet certain income requirements. Benefits programs typically require you to provide proof of income when you apply. Those income requirements also apply to the Medi-Cal program. In some cases, you might be eligible for Medi-Cal based on your income alone, even if you’re not signed up for another assistance program.
Medi-Cal income eligibility depends on the size of your household. To qualify for free Medi-Cal coverage, your income must align with 138% of the poverty level, based on the number of people who live in your home. The income limits based on household size are:
- One person: $20,783
- Two people: $28,208
- Three people: $35,632
- Four people: $43,056
- Five people: $50,481
- Over five people: Add $7,425 to the income limit for every person in a household above five people.

What Benefits Are Covered Under Medicaid in California?
When you go without health insurance, any cough, cold or injury can be a cause for concern. You might worry about how you’ll pay for health care when you need it. Fortunately, Medi-Cal takes the worry out of affording health coverage. The program provides coverage for preventive medical care and treatment when you’re sick or injured.
The Affordable Care Act requires qualified health plans, including Medicaid plans, to offer coverage of Essential Health Benefits, which include:
- Outpatient (ambulatory) services.
- Hospitalization.
- Emergency services.
- Maternity and newborn care.
- Mental health and substance abuse treatment services.
- Prescription medications.
- Physical and occupational therapy (or rehabilitative and habilitative services).
- Preventive and wellness services and chronic disease management.
- Dental and vision care.
If you’ve been putting off seeing a doctor or getting a treatment you need out of concern about its cost, getting coverage from Medi-Cal can help you take care of your health.
How Do I Know if I Qualify for Medicaid Services?
You can use a Medicaid calculator to verify your eligibility if you’re unsure whether you meet the Medicaid qualifications and income requirements. Simply enter your information, including your state or zip code, income, household size and the number of adults and children you want to enroll.
A Health for California agent can also help you determine your eligibility. Our agents will review your income information, family details and other relevant factors, such as your age and health, and help you put together your application.
How to Apply for Medi-Cal Benefits
Navigating Medi-Cal can feel overwhelming. Whether you are a first-timer or reapplying, here is how you can apply, cutting through the confusion to ensure you get the coverage you need:
- Gather the required documents: Get your proof of income, like pay stubs, tax returns or W-2 forms. Gather your proof of legal residency, an identification document like your driver’s license, and proof of address, like a lease agreement or utility bill.
- Apply in person or online: You can save time by applying online, going to your county’s Medi-Cal office or calling the service center for guided assistance.
- Wait for eligibility verification: You will receive a notification confirming your eligibility for Medi-Cal benefits. Prior to this, your county’s social services office may contact you to verify any additional information that helps process your application.
- Receive documents: You will receive a final notice of action to confirm if you qualify for Medi-Cal. If you qualify, you will get your BIC in the mail, allowing you to use the benefits at your disposal.
- Understand the timeline: Applications may take between 45 to 90 days to process. You can check your application’s status online or call your county office for more feedback.
Note that you need to renew your application annually to keep coverage, so keep your income and household information updated to avoid a lapse in coverage. That being said, Medi-Cal often offers retroactive benefits to cover past medical expenses within a specified time frame.
Plan Enrollment
At first, you will be covered under Medi-Cal’s Fee-for-Service. In some counties, you will then have 30 days to choose a health care plan, after which a plan will be chosen on your behalf. If you receive your health “welcome packet” in the mail, your health care plan was chosen automatically.
Apply for Medi-Cal With Health for California
Medi-Cal can be a lifeline for many families. By staying organized and proactive, you can navigate the system with confidence. Need more help? Our team guides Californians like you through all the affordable health care options, ensuring you find the coverage you need that fits your budget.
Health for California is here to help you determine your Medi-Cal eligibility. Our free agents are always available to answer your questions and get you a quote for your health care coverage. If you want to enroll yourself or your family in Medi-Cal, get your free quote today.